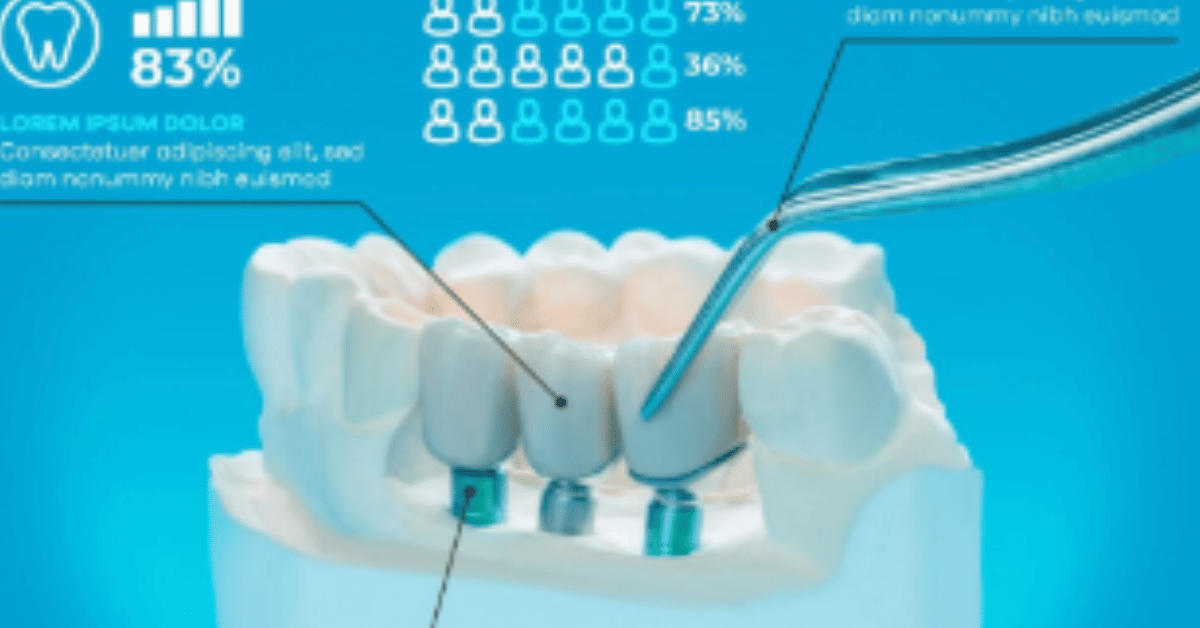
Molar teeth implants have emerged as a transformative solution for restoring chewing function, maintaining oral health, and preserving jawbone strength. When a molar is lost due to decay, trauma, or gum disease, the resulting gap does more than affect a smile — it impacts the efficiency of chewing and the structural integrity of the mouth. A molar teeth implant involves placing a titanium or zirconia post into the jawbone, serving as an artificial root, which is later topped with a custom-made crown. This procedure not only replaces the missing tooth but also stimulates the jawbone, preventing deterioration over time. For patients seeking a permanent, stable, and natural-looking alternative to dentures or bridges, molar teeth implants have become the gold standard. Unlike removable options, implants offer unparalleled stability and can last decades with proper care. This guide explores every aspect — from candidacy and procedure steps to aftercare and cost considerations — providing you with the clarity to make an informed decision about your oral health investment. As Dr. Elaine Porter, a leading prosthodontist, puts it, “A molar implant is not just a tooth replacement; it’s a restoration of function, health, and confidence.”
Understanding the Importance of Molar Teeth
Molars are the workhorses of the mouth, responsible for grinding and chewing food efficiently. Each side of the upper and lower jaw typically has two premolars and three molars, including the wisdom tooth. Losing one molar can shift the bite, force surrounding teeth to move, and cause jaw strain. Over time, these changes may lead to temporomandibular joint (TMJ) issues, gum recession, and increased tooth wear. A molar implant fills the gap with a prosthetic tooth rooted in the bone, preserving alignment and protecting the bite. Without timely replacement, the adjacent teeth may tilt or drift, causing difficulty in cleaning and raising the risk of cavities. Moreover, the loss of a molar compromises the distribution of chewing forces, leading to uneven wear on other teeth. Dental experts emphasize that molar implants maintain harmony in the oral structure while also supporting facial aesthetics, especially in the lower face where bone loss can cause visible sagging.
How Molar Teeth Implant Work
A molar implant replicates both the visible crown and the root of the tooth. The implant post, usually made of titanium for biocompatibility, is surgically placed into the jawbone. This post undergoes a process called osseointegration, where bone cells grow and fuse around it, securing it in place. After healing, an abutment connects the post to the custom crown, which is shaped and colored to match the surrounding teeth. Unlike bridges that rely on adjacent teeth for support, implants are standalone solutions, ensuring the integrity of neighboring teeth remains intact. This independence reduces long-term dental work and preserves natural enamel. Additionally, implants restore over 90% of natural chewing ability, far exceeding the performance of dentures. In the context of molars, which bear the greatest chewing load, this durability is essential. Patients often report that, after the adjustment period, the implant feels indistinguishable from a natural tooth. “An implant is a fusion of medical engineering and artistry,” says Dr. Marcus Lee, a dental implant specialist.
Types of Molar Teeth Implant
While the basic principle of replacing the tooth root with an artificial post is consistent, molar implants can vary in design, material, and placement technique. The most common is the endosteal implant, which is placed directly into the jawbone. Subperiosteal implants, used when bone density is insufficient, rest on top of the jawbone but beneath the gum tissue. For molars, wide-platform implants are often chosen to withstand the higher chewing pressure. Materials range from titanium — known for its strength and biocompatibility — to zirconia, which offers a metal-free, aesthetic alternative. Immediate-load implants allow the placement of a temporary crown on the same day, although these are typically used in specific conditions where bone stability is high. Patients with limited bone may require a two-stage process, sometimes combined with bone grafting. The choice depends on factors like jawbone health, bite alignment, and the patient’s preference for metal or ceramic materials.
Table 1: Common Types of Molar Teeth Implant and Their Characteristics
| Implant Type | Placement Method | Material Options | Typical Use Case | Healing Time |
|---|---|---|---|---|
| Endosteal Implant | Inside jawbone | Titanium, Zirconia | Standard molar replacement | 3–6 months |
| Subperiosteal Implant | On top of jawbone, under gums | Titanium | Low bone density without grafting | 2–4 months |
| Wide-Platform Implant | Inside jawbone (wider base) | Titanium | High load-bearing molar regions | 3–6 months |
| Immediate-Load Implant | Inside jawbone with temp crown | Titanium, Zirconia | Strong bone density cases, faster restoration | 0–3 months |
The Procedure: Step-by-Step Overview
The molar teeth implant procedure typically unfolds over several months, allowing for proper healing and integration. First, a comprehensive dental exam, including X-rays and 3D imaging, assesses bone health and oral structure. The dentist then develops a customized treatment plan. The surgical placement of the implant post is performed under local anesthesia or sedation. Following this, a healing period is necessary for osseointegration — often three to six months. Once integration is complete, a small connector called an abutment is attached, and impressions are taken for the final crown. The permanent crown is then fabricated in a dental lab and securely fitted. Throughout the process, temporary crowns or partial dentures may be used to maintain appearance and function. Post-operative care includes antibiotics, pain management, and strict oral hygiene to prevent infection. The step-by-step approach ensures long-term stability and minimizes complications.
Table 2: Molar Implant Procedure Timeline
| Stage | Description | Timeframe |
|---|---|---|
| Initial Consultation | Exam, imaging, treatment planning | 1–2 appointments |
| Surgical Placement | Implant post insertion | 1–2 hours |
| Osseointegration Period | Bone fuses with implant | 3–6 months |
| Abutment Placement | Connector attachment | 1–2 weeks healing |
| Crown Placement | Permanent molar crown fitted | 1–2 weeks |
Potential Risks and Complications
Like any surgical procedure, molar teeth implants carry certain risks, although success rates exceed 95% when performed by experienced professionals. The most common issues include minor swelling, bruising, and temporary discomfort following surgery. In rare cases, infection may occur if post-operative care is neglected. Failure of osseointegration, where the implant does not fuse with the bone, can happen due to insufficient bone density, smoking, or uncontrolled medical conditions like diabetes. Nerve injury is a risk if the implant is placed too close to a nerve channel, leading to tingling or numbness in the lips or chin, though such cases are uncommon. Sinus issues may arise when replacing upper molars if the implant protrudes into the sinus cavity. These risks are minimized through proper diagnostics, skilled surgical technique, and adherence to post-surgical instructions. Patients are advised to disclose all medications and health conditions before treatment to ensure the safest approach.
Benefits Beyond Tooth Replacement
The advantages of molar teeth implants extend far beyond simply filling a gap in your smile. Functionally, they restore natural chewing strength, enabling you to enjoy a full range of foods without restriction. Structurally, implants preserve bone density by stimulating the jaw in the same way natural roots do. This prevents the bone resorption that typically follows tooth loss, maintaining facial contours and preventing premature aging. Implants also reduce the strain on neighboring teeth, preventing them from shifting or wearing down prematurely. Aesthetically, the custom-designed crown blends seamlessly with natural teeth, often improving the appearance of the entire smile. Long-term, implants are more cost-effective than bridges or dentures, as they rarely need replacement when properly maintained. According to Dr. Linda Chen, “When we replace a molar with an implant, we’re not just restoring a tooth — we’re preserving oral health for decades.” This holistic benefit makes implants the preferred choice for many patients.
Ideal Candidates for Molar Implants
Not everyone is an immediate candidate for a molar teeth implant. Successful placement depends on having adequate bone volume and density to support the implant post. Patients with healthy gums, good overall oral hygiene, and no active periodontal disease tend to have the best outcomes. Age is less of a barrier than health status; older adults can be candidates if bone structure is sufficient. Those who smoke, have uncontrolled diabetes, or suffer from immune-compromising conditions may need additional evaluation or pre-treatment. In cases of bone loss, procedures such as bone grafting or sinus lifts can prepare the site for implant placement. It’s also important that the patient commits to consistent oral hygiene and regular dental visits. A strong willingness to follow care instructions plays a significant role in implant success. Dentists often stress that molar implants require not just financial investment but a personal commitment to long-term oral maintenance.
Pre-Surgical Preparation
Preparation for a molar teeth implant begins with a thorough dental and medical evaluation. The dentist will take detailed scans, often using cone-beam computed tomography (CBCT), to assess bone depth and proximity to nerves or sinuses. Blood tests may be recommended for patients with underlying health conditions. The pre-surgical plan will outline anesthesia type, surgical steps, and expected recovery time. Patients are often advised to avoid smoking, limit alcohol, and maintain a nutrient-rich diet in the weeks leading up to the procedure to promote healing. If bone grafting is required, this will be performed in advance, adding several months to the timeline. In some cases, infected tooth roots or damaged bone must be treated before implant surgery. Proper preparation minimizes risks and sets the stage for a smoother recovery. As a precaution, some dentists prescribe antibiotics prior to surgery to reduce infection risk, especially for patients with heart conditions or joint replacements.
Post-Surgery Recovery and Aftercare
Recovery from molar implant surgery typically involves mild to moderate discomfort for a few days, managed with over-the-counter pain medication or prescribed analgesics. Swelling peaks within 48 hours and gradually subsides. Ice packs, soft foods, and saltwater rinses help promote healing. Patients should avoid hard, crunchy, or sticky foods for at least two weeks to protect the surgical site. Brushing near the implant should be gentle at first, but maintaining cleanliness is crucial to prevent infection. Smoking should be avoided entirely during the healing period, as it significantly increases the risk of implant failure. Most patients return to work within a day or two, depending on the complexity of the procedure and their comfort level. Follow-up appointments are scheduled to monitor healing and check for proper osseointegration. Long-term care involves regular dental cleanings and checkups, along with daily flossing and brushing to keep surrounding gums and bone healthy.
Cost Considerations and Insurance Coverage
The cost of a molar teeth implant can vary widely depending on location, dentist expertise, materials used, and whether additional procedures like bone grafting are necessary. In the United States, the average price for a single molar implant ranges from $3,000 to $6,000, including the implant post, abutment, and crown. Zirconia crowns and premium implant systems can increase the price further. Dental insurance rarely covers the full cost but may provide partial reimbursement, particularly if tooth loss resulted from an accident or medical necessity. Some plans cover the crown portion but not the surgical placement. Financing options, including payment plans and healthcare credit lines, are often available through dental offices. Patients are encouraged to obtain detailed treatment estimates and confirm insurance benefits before proceeding. While the upfront investment is significant, the long-term durability and reduced maintenance costs often make implants more economical than alternatives like bridges, which may need replacement every decade.
Technological Innovations in Molar Teeth Implant
Recent advancements in dental implant technology have improved both success rates and patient comfort. Computer-guided surgery allows for highly precise placement, reducing the risk of nerve damage or sinus complications. New surface treatments on titanium implants enhance osseointegration speed, shortening recovery times. Digital impressions replace messy traditional molds, enabling faster and more accurate crown fabrication. Zirconia implants have gained popularity for patients seeking metal-free solutions with excellent aesthetics. Some systems now feature platform-switching designs, which help preserve gum tissue and bone around the implant neck. Additionally, minimally invasive flapless techniques reduce surgical trauma and speed healing. Artificial intelligence is also beginning to influence implant planning by predicting optimal placement angles and load distribution. These innovations not only improve functional outcomes but also enhance the overall patient experience, making molar implant procedures more accessible and efficient than ever before.
Long-Term Maintenance and Care
Molar teeth implant are designed to last for decades, but their longevity depends heavily on proper care. Daily oral hygiene routines should include brushing twice a day with a soft-bristled toothbrush and flossing around the implant using specialized floss or interdental brushes. Avoiding excessive force from teeth grinding (bruxism) is important; patients prone to grinding may need a custom night guard. Regular dental visits, ideally every six months, allow early detection of potential issues like peri-implantitis — an inflammatory condition similar to gum disease that can compromise implant stability. A balanced diet rich in calcium and vitamin D supports bone health, while limiting sugary snacks reduces the risk of surrounding tooth decay. Importantly, molar implants are resistant to cavities but not immune to gum problems, so diligent care is essential. As one implant specialist notes, “Think of your implant like a luxury car — built to last, but only if you maintain it.”
Comparing Molar Teeth Implant with Alternatives
When considering tooth replacement, it’s important to weigh implants against other options such as bridges and dentures. Fixed bridges involve shaving down adjacent teeth to support the prosthetic tooth, which can weaken healthy enamel over time. Removable partial dentures are less invasive and more affordable but offer reduced stability and comfort, particularly in the back of the mouth where chewing forces are greatest. Molar implants, by contrast, do not impact neighboring teeth and offer superior chewing performance. The initial cost is higher, but over the long term, implants often prove more cost-effective due to their durability and lower maintenance needs. Patients who value both function and aesthetics generally find implants the most satisfying choice. However, those with severe bone loss or health conditions that complicate surgery may opt for alternatives. The decision should always be based on a thorough discussion with a qualified dental professional who understands the patient’s priorities and constraints.
Psychological and Lifestyle Impact
Beyond the technical and functional aspects, molar implants can have a profound psychological benefit. Many patients report an increase in confidence when eating in public or speaking, knowing their replacement tooth is secure. The ability to chew properly allows for a more varied and enjoyable diet, improving overall nutrition. This in turn can boost energy levels and general well-being. Socially, implants eliminate the worry of dentures slipping or food becoming trapped, allowing for more carefree interactions. For younger patients, the stability of an implant helps maintain jaw structure over decades, avoiding the aged appearance sometimes caused by bone loss. The combination of physical restoration and emotional reassurance makes molar implants one of the most rewarding dental investments available. Dentists frequently observe that patients who undergo the procedure often wish they had done it sooner, citing improved quality of life as the most significant outcome.
Conclusion
Molar teeth implant stand at the intersection of medical science, engineering precision, and aesthetic artistry. They restore not just a tooth, but the intricate balance of the mouth, preserving chewing ability, jawbone health, and facial structure. While the procedure requires financial investment and personal commitment, the rewards — functional, aesthetic, and psychological — often outweigh the costs. From the initial consultation to long-term maintenance, the process reflects the remarkable advancements in modern dentistry. For those with missing molars, an implant can be life-changing, providing a permanent, natural-feeling solution that enhances both health and confidence. As dental technology continues to evolve, the success rates and accessibility of molar implants will only improve, offering more people the chance to reclaim the comfort and joy of a fully functional smile. In the words of Dr. Porter, “Replacing a molar is not just fixing a tooth — it’s restoring the foundation of your bite, your health, and your smile.”
FAQs
1. How long do molar teeth implants last?
With proper care, molar implants can last 20 years or more, and many remain functional for a lifetime. Their durability depends on factors such as oral hygiene, regular dental checkups, and avoiding habits like smoking or teeth grinding. Unlike bridges or dentures, implants integrate with the jawbone, making them one of the longest-lasting tooth replacement options available.
2. Is the molar implant procedure painful?
The surgery is typically performed under local anesthesia or sedation, so discomfort during the procedure is minimal. After surgery, patients may experience mild soreness or swelling, which usually subsides within a few days and can be managed with prescribed or over-the-counter pain relief. Most people find the process far less uncomfortable than they initially feared.
3. How much does a molar tooth implant cost?
In most regions, the cost for a single molar implant — including the post, abutment, and crown — ranges from $3,000 to $6,000. This cost can increase if bone grafting or advanced imaging is required. While dental insurance often does not cover the entire amount, many plans offer partial benefits for specific components.
4. Can anyone get a molar implant?
Not everyone is an immediate candidate. Good overall health, healthy gums, and adequate jawbone density are essential for successful placement. Patients with bone loss can still receive implants after preparatory treatments such as bone grafts or sinus lifts. A detailed evaluation by a dental implant specialist determines suitability.
5. How soon can I eat normally after a molar implant?
Patients typically start with soft foods for the first week after surgery, gradually reintroducing firmer textures as healing progresses. Full chewing ability is restored once the implant has fully integrated with the bone and the permanent crown is placed, usually within 3–6 months.