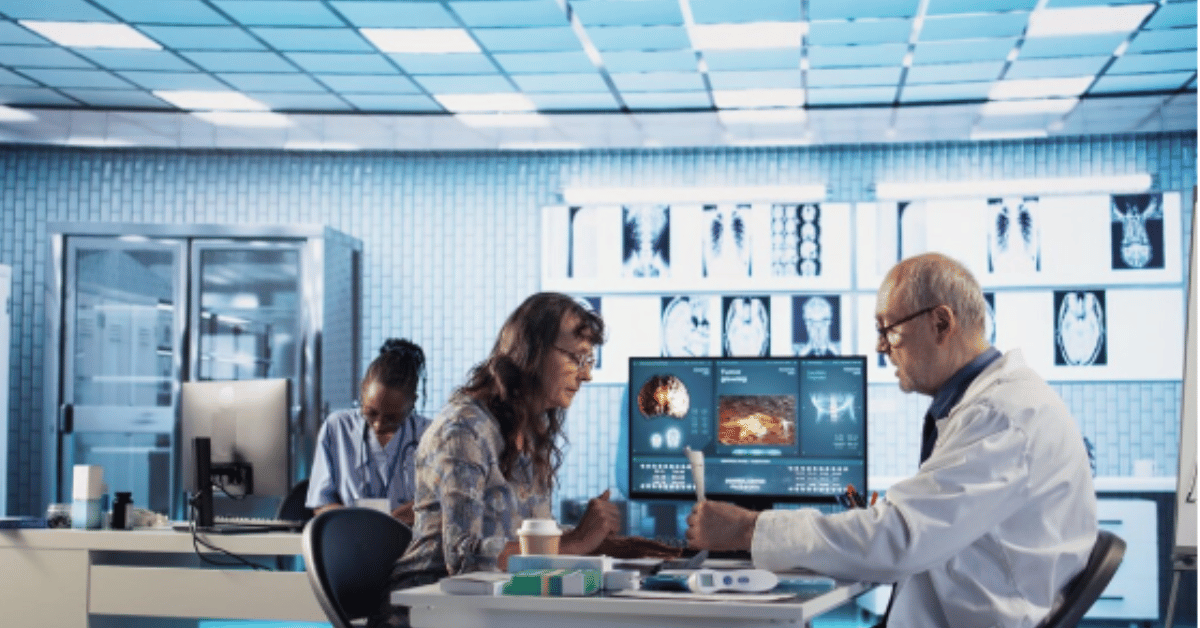
NGS Connex has become an increasingly referenced term in the healthcare and medical services sector, yet for many people outside professional circles, its precise role and value may remain somewhat obscure. In simple terms, NGS Connex is an advanced online platform designed to facilitate communication and streamline processes between providers, patients, and payers. It operates as a digital bridge that connects health systems with insurers, ensuring that claims, authorizations, and clinical data are managed more efficiently. For anyone searching to understand what NGS Connex truly is, the most essential point is that it is not a medical treatment or device itself—it is a technological infrastructure that makes healthcare delivery smoother and more reliable. Within the first moments of interaction, NGS Connex aims to reduce paperwork, shorten approval times, and enhance collaboration across multiple stakeholders in the medical industry.
The growing reliance on NGS Connex represents a broader shift toward digital integration in healthcare, where efficiency and data integrity are critical to patient care and financial management. Similar to how electronic banking reshaped personal finance, platforms like NGS Connex are transforming the way medical providers and insurers interact, minimizing errors while enabling faster decisions. This guide provides a comprehensive exploration of its purpose, architecture, benefits, and limitations, with a focus on why it is now regarded as indispensable in the ever-evolving healthcare system. We will examine how it impacts providers, what patients should know about its role, the industries that benefit most, and the technical backbone that supports it. By the end of this article, readers will gain a full appreciation of why NGS Connex matters today and how it is shaping tomorrow’s healthcare landscape.
What is NGS Connex?
NGS Connex stands for National Government Services Connex, a secure online web portal primarily used in the healthcare sector for processing Medicare and insurance claims. It was initially developed to provide an easier way for medical professionals and administrators to check claim status, eligibility, and payment details without relying on cumbersome manual methods. The system enables real-time access to essential information, thereby saving time for both providers and insurers. By offering a centralized platform, NGS Connex removes redundancy, allowing different healthcare entities to collaborate with minimal delays.
At its core, NGS Connex is not just a digital filing cabinet; it is a dynamic communication hub. Providers can log in, verify patient benefits, submit claims, and receive notifications about updates instantly. Insurers benefit by ensuring compliance, maintaining regulatory requirements, and reducing instances of fraud or duplicate claims. Patients indirectly experience its benefits because approvals and reimbursements happen faster, which can significantly reduce stress during already challenging healthcare experiences.
One of the reasons NGS Connex is so valued is that it balances technical sophistication with user accessibility. Unlike older claim management systems that demanded specialized training, NGS Connex is relatively intuitive, with dashboards, reports, and forms designed for efficient navigation.
Historical Development of NGS Connex
The roots of NGS Connex can be traced back to the early 2000s when healthcare providers were struggling with fragmented communication tools and inconsistent claim processes. National Government Services, a Medicare administrative contractor, recognized the urgent need for a streamlined system that could integrate technology with regulatory compliance. The result was Connex, which quickly gained traction as a standard platform for interacting with Medicare systems.
Initially, its features were limited to eligibility verification and claim status checks, but subsequent updates expanded its capabilities. Over the years, functionalities such as prior authorization requests, electronic remittance advice, and interactive dashboards were added. Each enhancement was designed with the intent to reduce inefficiencies in communication between providers and insurers.
By the mid-2010s, NGS Connex had evolved into a robust portal serving thousands of providers across multiple states. Its integration with Medicare systems ensured not only smoother processes but also better data tracking and reporting for compliance. This historical trajectory illustrates how necessity, regulation, and technology converged to create a platform that would become central to healthcare administration.
Core Functions of NGS Connex
NGS Connex is built around a set of core functions that cater to different stakeholders in the healthcare ecosystem. These functions include:
- Eligibility Verification – Providers can instantly check whether a patient qualifies for certain services or treatments under Medicare or other insurance.
- Claim Submission and Tracking – Submitting claims digitally reduces errors and enables providers to track progress in real time.
- Prior Authorization Requests – Streamlining the process of gaining insurer approval for treatments before they occur.
- Payment Details and Remittance – Providers can view payment breakdowns, adjustments, and remittance advice without waiting for paper documentation.
- Appeals and Adjustments – NGS Connex also facilitates the process of appealing denied claims or making necessary adjustments.
These core functions reflect its purpose: simplifying complex administrative processes in healthcare. Each element is structured with compliance in mind, ensuring providers adhere to strict Medicare guidelines while still benefiting from technological efficiency.
Benefits of NGS Connex for Healthcare Providers
Healthcare providers are among the primary beneficiaries of NGS Connex. In a system often burdened by bureaucracy, the platform introduces much-needed clarity and speed. For instance, eligibility verification allows providers to avoid the costly mistake of delivering services that are not covered. Similarly, claim tracking ensures transparency by allowing providers to monitor exactly where their submissions stand, whether pending, approved, or denied.
One of the most significant advantages is reduced administrative cost. Instead of hiring additional staff to manage manual paperwork, providers can rely on automated features. This cost reduction does not just benefit clinics and hospitals but also trickles down to patients in the form of fewer billing errors and quicker resolution of issues.
NGS Connex also supports compliance, an often overlooked but critical factor in healthcare. By adhering to Medicare’s evolving regulations, providers can avoid penalties and ensure consistent quality in their reporting. The ability to appeal denials directly through the platform also saves providers from lengthy back-and-forth exchanges.
Benefits of NGS Connex for Patients
While patients may not directly log in to NGS Connex, its impact on their healthcare journey is significant. Faster claim processing means fewer delays in treatment approvals, particularly for procedures requiring prior authorization. This can be life-changing for individuals awaiting critical surgeries or therapies.
Patients also benefit indirectly through improved accuracy. By minimizing claim errors, the platform reduces the risk of unexpected bills or coverage issues. Moreover, with providers spending less time on administrative work, they can dedicate more focus to patient care. As one healthcare administrator once said, “The less time we spend chasing paperwork, the more time we can spend at the bedside.”
Additionally, patients are spared the frustration of repeated delays, as claims and approvals can now be processed within days instead of weeks. The sense of security that comes from knowing that their provider is supported by a reliable system is an intangible yet powerful benefit.
Comparative Table: Providers vs Patients Benefits
| Stakeholder | Key Benefits of NGS Connex | Impact Level |
|---|---|---|
| Providers | Reduced admin costs, compliance support, claim tracking, appeals process | High |
| Patients | Faster approvals, reduced billing errors, better care focus from providers | Moderate to High |
Technical Architecture of NGS Connex
The technical backbone of NGS Connex is designed with security, scalability, and compliance at its forefront. It operates on a secure web-based infrastructure, ensuring that data exchange between providers and insurers remains encrypted and compliant with HIPAA standards. Its modular design allows for updates without requiring system overhauls, meaning new features can be integrated seamlessly.
User authentication protocols ensure that only authorized individuals can access sensitive data. Multi-factor authentication has been implemented in recent versions, reducing risks of unauthorized access. Additionally, the platform is cloud-based, enabling scalability as more providers adopt it. This design choice also allows for higher uptime reliability, ensuring providers can access it even during peak demand.
The system’s interface is another strength. Built with user experience in mind, it employs dashboards, color-coded status updates, and intuitive navigation to simplify complex processes. By making technology accessible, NGS Connex bridges the gap between technical sophistication and practical usability.
Challenges and Limitations of NGS Connex
Despite its many benefits, NGS Connex is not without limitations. One of the most common challenges reported by users is system downtime, which can temporarily halt claim submissions or status checks. While these instances are rare, they highlight the reliance providers place on its availability.
Another limitation lies in user training. Although the interface is designed to be user-friendly, staff must still undergo training to fully utilize all features. Smaller clinics with limited resources may find this transition more difficult.
There are also concerns about data overload. With so much information available, providers must develop strategies to manage and prioritize what is most important. Finally, while NGS Connex supports Medicare claims effectively, integration with private insurance systems may not always be seamless, creating gaps for providers who deal with multiple payers.
Future Prospects of NGS Connex
Looking ahead, NGS Connex is expected to evolve alongside broader healthcare digitalization trends. Artificial intelligence could play a role in automating claim approvals, reducing manual intervention even further. Predictive analytics may help identify patterns of fraud or inefficiency, saving billions in potential costs.
Interoperability will also be a key area of focus. The ability for NGS Connex to integrate more effectively with private insurers and electronic health record (EHR) systems will determine its long-term value. As one industry expert put it, “The future of healthcare is in connectivity, and platforms like NGS Connex are the connectors.”
Expansion beyond Medicare is also a possibility, as the principles of streamlined communication and compliance are universally valuable. If adopted by broader insurance networks, NGS Connex could redefine claim management across the healthcare landscape.
Table: Challenges vs Future Solutions
| Current Challenges | Proposed Future Enhancements |
|---|---|
| Occasional downtime | Cloud redundancy and backup systems |
| Training needs | Interactive AI-driven tutorials |
| Data overload | Advanced analytics and prioritization tools |
| Limited integration | Improved interoperability with private insurers and EHRs |
Conclusion
NGS Connex represents more than just a digital portal—it is a transformative infrastructure that has reshaped how healthcare providers, insurers, and patients interact. By offering streamlined claim processing, eligibility verification, prior authorizations, and compliance support, it has reduced inefficiencies that once plagued the healthcare system. Providers save time and costs, patients receive faster approvals, and insurers benefit from reduced errors and fraud prevention.
At the same time, challenges such as training requirements and integration gaps remind us that no system is perfect. Yet, the trajectory of NGS Connex indicates a strong future. With potential integration of AI, expanded interoperability, and enhanced reliability, it is poised to play an even greater role in healthcare’s digital transformation.
In the words of a healthcare leader, “Efficiency in healthcare administration may not cure diseases, but it creates the conditions where cures can happen faster.” NGS Connex embodies this philosophy by ensuring that while doctors and nurses focus on saving lives, the system supporting them runs smoothly, quietly, and effectively. For anyone seeking to understand its significance, the answer is clear: NGS Connex is not just a tool—it is an essential partner in modern healthcare.
FAQs
1. What is NGS Connex primarily used for in healthcare?
NGS Connex’s primarily used as a secure web-based platform for healthcare providers to verify patient eligibility, submit and track claims, manage prior authorization requests, and review payment details. It simplifies communication with Medicare and ensures compliance with federal regulations, making it an essential tool for providers seeking efficiency and accuracy in claim processing.
2. Can patients directly access and use NGS Connex?
No, NGS Connex’s not designed for direct patient use. Instead, it functions as an administrative and operational portal for providers and insurers. Patients benefit indirectly by experiencing faster approvals, fewer billing errors, and improved coordination of care, but they do not interact with the platform themselves.
3. How secure is the NGS Connex platform for sensitive healthcare data?
NGS Connex’s built with robust security measures, including HIPAA compliance, encrypted communication, and multi-factor authentication protocols. These protections ensure that sensitive patient and provider information is safeguarded from unauthorized access while maintaining strict adherence to healthcare privacy standards.
4. What challenges do providers face when adopting NGS Connex?
Some of the challenges include initial training requirements for staff, occasional system downtime, and potential data overload due to the vast amount of available information. Smaller clinics may also find the learning curve steeper, but once implemented, the system offers significant long-term advantages in efficiency and cost savings.
5. What future developments are expected for NGS Connex?
Future developments are likely to include deeper integration with electronic health records (EHRs), greater interoperability with private insurers, and the introduction of AI-driven tools for claim automation and fraud detection. These advancements aim to further reduce administrative burdens and create a more seamless healthcare ecosystem.